2376-0249
Clinical-Medical Image - International Journal of Clinical & Medical Images (2022) Volume 9, Issue 9
Author(s): Jihane EL Houssni*, Siham Oukacem, Yahya El Harras, Nada Adjou, Meryem Edderai and Jamal El Fenni
Department of Radiology, Mohammed Vth military hospital, Ryad Street, 10010 Rabat, Morocco
Date of Submission: 12 September, 2022, Manuscript No. ijcmi-22-77733; Editor assigned: 13 September, 2022, 2022, PreQC No. P-77733; Reviewed: 19 September, 2022, QC No. Q-77733; Revised: 22 September, 2022, Manuscript No. R-77733; Published: 30 September, 2022, DOI: 10.4172/2376-0249.1000849
Citation: Houssni JE, Oukacem S, Harras YE, Adjou N and Edderai M et al. (2022) Acute Spinal Cord Infarction: A Case Report. Int J Clin Med Imaging 9:849.
Copyright: © 2022 Houssni JE, et.al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Clinical history
A 62-year-old man without previous pathologic antecedents was admitted to the emergency department for sudden-onset quadriplegia.
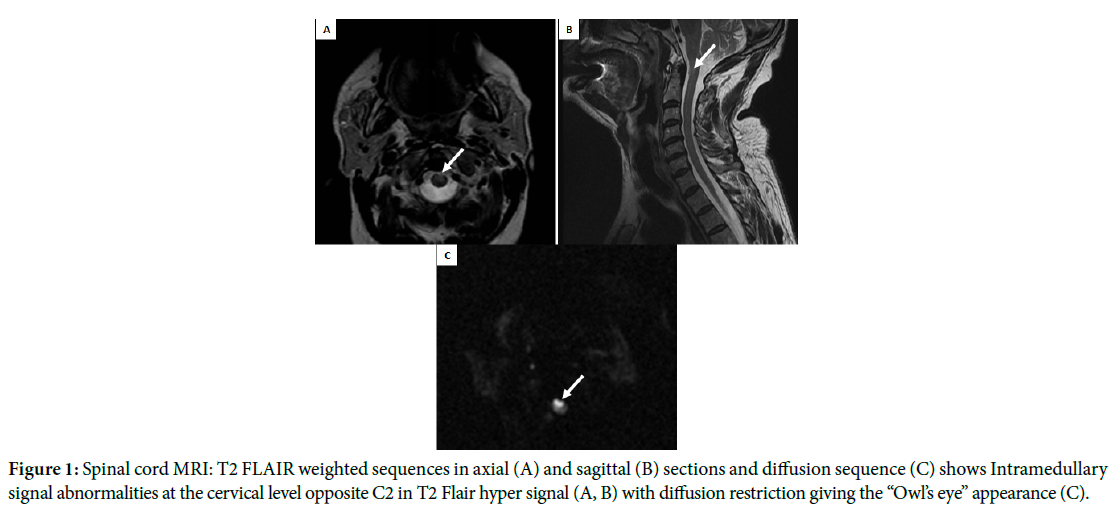
Spinal cord MRI: T2 FLAIR weighted sequences in axial (A) and sagittal (B) sections and diffusion sequence (C) shows Intramedullary signal abnormalities at the cervical level opposite C2 in T2 Flair hyper signal (A, B) with diffusion restriction giving the “Owl’s eye” appearance(C) (Figure 1).
Spinal cord ischemia is a rare entity with a poor prognosis [1]; it represents about 6% of all acute myelopathies and about 1 to 2% of all vascularneurological pathologies [2]; it occurs mainly in patients with a cardiovascular background disease [1].
The onset of symptoms is usually abrupt [3], and the clinical presentation depends mainly on the location and extent of the infarction [1,3]. Anterior Spinal Artery Syndrome is the most common; it usually presents as a bilateral loss of motor function and pain/temperature sensation, with relative sparing of proprioception and vibratory senses below the level of the lesion [1]. MRI is the crucial modality in case of suspected acute spinal cord ischemia [3]; it presents as a restriction of diffusion imaging of the spinal cord, hyper intense signal in T2 and STIR, and iso intense signal in T1 [1], a variety of characteristic MRI “signs” have been described:
• Pencil-like: Zone of signal abnormality at the site of ischemia in sagittal T2-weighted MRI [2].
• Sagittal T1-weighted imaging may show segmental cord swelling or focally elevated signal thought to represent haemorrhagic transformation [2].
• Owl’s eye sign: Symmetrical T2 hyper signal abnormality of the anterior horn neurons, very suggestive of the anterior spinal syndrome [2].
• Positive anterior cauda sign: characteristic of thoracolumbar spinal cord ischemia, it translates into an asymmetric enhancement of the anterior nerve roots of the cauda equina [2].
• Compressive myelopathy: Extra spinal tumor, hematoma, abscess, herniated disc
• Infectious myelopathy: HTLV1, HIV, varicella, progressive multifocal leuko encephalopathy (PML)
• Inflammatory or autoimmune myelopathy: transverse myelitis, multiple sclerosis, systemic lupus erythematosus, Devic’s syndrome
• Others: neuromyelitis optica, arteriovenous malformations, porphyria.
Spinal cord infraction; MRI; Owl’s eye sign
[1] Vargas MI, Gariani J, Sztajzel R and Barnaure-Nachbar I et al. (2015) Spinal cord ischemia: practical imaging tips, pearls, and pitfalls. Am J Neuroradiol 36(5): 825-830.
Google Scholar, Crossref, Indexed at
[2] Caton MT, Huff JS. (2021) Spinal Cord Ischemia. StatPearls Publishing.
[3] Mohr JP, Wolf Philip A, Grotta James C and Moskowitz Michael A et al. (2011) Spinal Cord Ischemia. Stroke (Fifth Edition) 643-657.
sushihouse kolstads americanpridefasteners trueforge hotelposeidon youngswoodfinishing arditomason thebestofreno eeclongisland doktervanhecke famsales adla bogatylaw prefplastics kirbycontractinginc unlsp boban dottoressaromolimonica thebestofsanfrancisco vernix digitaldocuments tristatepropertybrokers sotrafib cemcorpny agenziaimmobiliarebuti joesitalianfoodmarket corpoguardiedicitta icsatc antoniniassicurazioni besel strappedincarseatsafety drevobeton blessingconstructionny centre-endorphine qmbtunisia elearning 357 mpress rrappliance ciaautomazioni antikva stubbanvel tacticalpublicrelations mpulshnk paulyboybrand lordshoes ijd-procom thebestrestaurants atkpalvelut ceat leonfukspc pilotexamssa ashgrovecabins universalshielding thebestofcharlotte johnjmazurinc rollnroaster thecabinetwarehouse pocketchangeduo thebestofmilwaukee resan sooli vwe centralwindowcleaning reinforcedplasticslab bugbustersofli ciandrigiardini arfada centrumeigenwijs thebestofmemphis maisonpearly islipll dcgraphicsinc agetranquille relisandroth thebestofcharleston traiteur-wn safi-ingenierie justmyvoice harrishardware louisbarbatolandscaping brightstartoursworld rga-insurance calacatajumper ezantia mrcheapocds van4holiday cigap richtour fagyhatar sicc weshopmall ventovuori sobatrapcapbon unityrubberllc thebestofsaltlakecity ircinc sescoindustries connply storen-servicesenter psnry greatneckcollision ironfitendurance tuscanycountryhouse sansovinocalcio bbradydesign samsam vdtarification springersoil thebestofdayton milantechnology labradoodlesoflongisland daliamohamed theconsultantpowerhouse gunnbrush kruunuosk shulmanproduce balcosupply conso-med federalnetworks bellmoreglass alwaysaffordableconcrete jayteeinsurance carolina-cabins cmorfinance stretchritepackaging dishaairwaysenterprise biocontrol distribio peterivill lcc inspekta jvidesigns royalroseinc calabriapizza fadhila prato-pronto-effetto arbemachine olsonelectricnj tkbl tuttifotokft alpernmd ggsupplywholesale almaxcorporation sotuflex ecustomgutter studenipotok metal-lineconcept rettsodontologi nutecsystems aclotbeach gjonnes-bygg cavalierinternational mnemos southfloridashuttles ajchemicalsupply rachelsfireisland concepto nesponge ultimatestylesofamerica techniquesmadeeasydrivingschool stevesmeatsfreeport eastwest gritbrush plussplan biosens viltkam wikaya paintballconcept justmyvoice securecarkeysupply justmyvoice allcountylegal catt plugandcharge ttandlcontracting justmyvoice islandboatlettering gms-tunisie sportsiena bloeiop touchofclasscollision kotekservice ittoscana pallongislandlacrosse industrialfinishings painoutband rakvag-batforening konemies rrfamilychiropractic infienile shbcgroup footpharmacydirect scuolaguidaprato ans-nettoyage autoskola saafa autolaky1 fixcars longislandelitelandscaping rayscan palaconstruction studio44 crealhome viniferi gavinburke ciprianigiardini davidpokorny osteriailcapodaglio thebestoffairfax centroorafofaccioli ateliervb bbdps thebestoffresno prodigus stratpak umisushirestaurant sotim suldalrenovasjon amer-equip k-kleven jerryspridepotatoes neuroky psicologozampoli jjslandscaping thebestofoklahomacity responsivesales paratie-antiallagamento-shop hearproof cfat ruspinameubles planetbioplastics lynbrook-plumber fcdf-ye brechanparkett valley-stream-plumber diagnosismaker aquavaria jedit garageennour heimdalbygg thebestoflittlerock raybomarine bayshorepaper gmstowing potatura-abbattimento-piante thebestoflouisville michaelalbert thebestofannarbor unitypavers mtnfueloil durub-mudiya lesgensdere dormerking thusney italianvistatravel maiemad gtiuniformcleaning suddenimpactli levituuli sourisalavie mayoiltank mschwartzfeather rands arieslimousines orthoticworld longislandcocktailhours waterjet allislandpaving dukediagnostic klfgoteborg yanezviaggi apruk decogato springeroilltd semapsolar irisgioiellicomprooro msedpsoftware fourcmanagement holemans 7consulting medinet evertile robertwitcomblandscape ceramics adrobotengineering volt-energy huisjacobs chimneyserviceboston eastmainstdental gcbt rememberingbriank elligiardiniespurghi paulslandscaping luisrestorations mgstunisie fixcarsny crcdd hotelprincipessalucca turvahallinta ralphjr thales irrigazione-giardini spantecsystems biomedic fgt-trading sols-egypt spectrumlaboratoriesinc prosecurite spongewarehouse afsainc dellafrancadevelopmentgroup leragazzedifirenze ferrettiwatches dovreentreprenor digitalhvac mostlymica fleurs-velghe autoscuolalebadie interlockingrubbertiles meadowcreekhoa bcn corpjetsupport jrkitchensflooring arteletti
 Awards Nomination
Awards Nomination