2376-0249
Clinical-Medical Image - International Journal of Clinical & Medical Images (2023) Volume 10, Issue 7
Author(s): Mohamed AI Amine EI Mouden*
Department of Surgery, Abdelmalek Essaadi University, Tangier, Morocco
*Corresponding Author:
Mohamed AI Amine EI Mouden
Department of Surgery
Abdelmalek Essaadi University
Tangier, Morocco
Tel: +212 45250071
E-mail: amine-528@hotmail.com
Received: 24 June 2023, Manuscript No. ijcmi-23-103713; Editor assigned: 26 June 2023, Pre QC No. P-103713; Reviewed: 14 July 2023, QC No. Q-103713; Revised: 18 July 2023, Manuscript No. R-103713; Published: 25 July 2023, DOI:10.4172/2376-0249.1000904
Citation: Mouden MAAE. (2023) Can we avoid a Protective Stoma and Improve Functional Results after Surgery for Rectal Cancer? Reinforced and Delayed Colo-Anal Anasftomosis: A New TecThnique Observaftional Sftudy abouft 5 Cases. Inft J Clin Med Imaging 10: 904.
Copyright: © 2023 Mouden MAAE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Colorectal cancer is a common cancer, accounting for nearly 10% of all cancers (Source: Globocan 2020) and ranking first among digestive cancers. More specifically, cancer of the rectum represents between 30% and 40% of colorectal cancers. Its treatment is mainly based on a surgical approach, but this could potentially lead to functional troubles, particularly digestive, urinary and sexual, as well as psychological side effects, especially if the body image is altered by an ostomy, even if temporary. Preservation of anal sphincter function is the main issue in this surgery, especially for cancers of the lower rectum, for which a colo-anal anastomosis is often necessary to meet the carcinological requirements of mesorectal resection, but with often mixed functional results [1-4]. Specifically with the aim of avoiding a protective stoma and improving functional results after colo-anal anastomosis we propose a modification of the colo-anal anastomosis technique, which will be performed in two stages with sphincter reinforcement, which has been nicknamed delayed and reinforced colo-anal anastomosis. This article aims to describe this new surgical procedure and to evaluate the first functional and surgical results.
The study is of an observational and descriptive nature and will run for two years, from January 2019 to December 2020.
Inclusion criteria:
• Patients with adenocarcinoma of the lower rectum within 6 cm of the anal margin confirmed by digital rectal examination and rigid rectoscopy plus biopsy.
• Patients who have received their radio-chemotherapy sessions according to the classic protocol (50 Gy divided into 25 sessions over a period of 5 weeks) or the short protocol (25 Gy in 5 days).
• Patients re-evaluated by CT-PET and pelvic MRI.
• Patients with a preserved anal sphincter based on MRI and DRE data.
All patients were informed of the experimental nature of the study and signed a consent form.
Evaluation criteria
• The possibility of avoiding a protective stoma.
• Assessment of anal continence according to the KIRWAN classification [5].
• Assessment of the degree of satisfaction in these patients.
Monitoring modality
• One consultation every month for 3 months.
• Then a consultation every three months for the first year.
• Then a consultation every 6 months during the second year.
First surgical step
Preoperative management of patients: The surgical procedure is performed between 8 and 10 weeks after the last course of radiotherapy. A macrogol-based colonic preparation is started 3 days before the surgery. The last 24 hours before surgery the colonic preparation is stopped by allowing a diet in the form of boiling water.
Surgical technique
All patients were operated on laparoscopically, under general anesthesia (GA) in the supine position, with the left arm at the side of the body and the legs spread. The main operator was positioned on the right of the patient, the first assistant on his left and the second assistant between the patient’s legs. The first operation consists of the creation of a pneumoperitoneum by open coelio with the introduction of a first 10 mm trocar above the umbilical which serves as a trocar for the 30° optic camera. A second 10 mm trocar is introduced in the right iliac fossa and a third 5 mm trocar in the right flank and a 5 mm trocar in the hypogastric area.
Abdominal time
After exploration of the abdominal cavity for peritoneal carcinosis or liver metastases, the surgical procedure is started by tilting the greater omentum upwards over the transverse colon and pushing the entire bowel to the right by adjusting the position of the operating table with a roll to the right and a Trendelenburg position, which allows the entire left mesocolon, Treitz’s angle and the promontory to be exposed downwards. Ligation of the inferior mesenteric artery is done 1 cm from its origin preserving inferior mesenteric and hypogastric innervation at this level. The inferior mesenteric vein is transected at the left edge of the D4. This vein may not be transected if section of the left superior colonic artery and vein allows sufficient lowering of the colon to the perineal region. Mobilization of the left colonic angle is carried out from the inside outwards through Toldt’s fascia under the inferior mesenteric vein, taking particular care not to injure the lower edge of the pancreas and after individualization of the ureter.
Pelvic time
Extra-fascial posterior, anterior and lateral dissection of the rectum allowing total resection of the mesorectum.
Perineal time
• Tumour resection
• The last operative step is the perineal step where the anal margin is exposed and the rectal mucosa is cut 1 cm below the lower pole of the tumour, preserving as much as possible the ilio-pectineal line and carrying out the dissection upwards until it joins the dissection plane carried out by laparoscopy.
• The surgical specimen is extracted trans-anally.
• Making a musculoserosal flap
After colonic sectioning 20-25 cm upstream of the tumour, an 8 cm long colonic segment is removed from the healthy part of the colon.
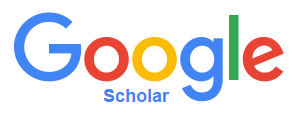
The sectioned colonic segment is stripped of its epiploic fringes, then incised vertically to obtain a rectangle (Figure 1), then stripped of its mucosa and submucosa, leaving only a musculoserosal flap by scraping with a scalpel blade. The flap is then placed in a cup containing saline.
The musculoserosal sleeve is obtained by folding the musculoserosal flap over itself, which is then fixed by separate stitches with 3/0 absorbable sutures. The muscular side is on the outside (Figure 2).
• Making a pericolic sleeve
The next step consists of applying this musculoserosal sleeve 5 cm from the distal part of the lowered colon, taking care to pass it over Riolan’s arch and in contact with the colonic wall and making it go around the lowered colon one and a half times (Figures 3a and 3b) and calibrated around a Foley catheter 16fr.
• Performing the colo-perineal anastomosis
Finally, the last operation consists of performing a colo-perineal anastomosis in the manner of a perineal stoma by invaginating the end of the lowered colon and fixing the perineal stoma by separate stitches with 3/0 absorbable thread (Figure 4).
• We did not perform a protective stoma in all patients
Post-operative management of patients: All patients received thrombo-prophylaxis based on low molecular weight heparin in preventive dose and early and progressive reintroduction of food as well as early mobilization from the first postoperative day of the patient. In addition to the classic daily postoperative clinical examination, particular attention will be paid to the appearance and coloring of the anastomosed colon at the perineal level. Irrigation with warm saline is performed from the second postoperative day onwards in all patients. The equipment used for this irrigation is a Foley catheter and a 50 cc syringe or an adapted irrigation system. Irrigation is started with 200 cc of lukewarm water on the first day, then 200 cc/day is added up to 1 to 1.5 liters/day. The frequency is set at one irrigation every 24 hours. Patients can be discharged from the 3rd postoperative day on condition that the technique of colonic irrigation is well assimilated by the patient himself or by a member of his family.
Second stage of surgery: Performing a colo-anal anastomosis
On an outpatient basis and on the tenth postoperative day. The patient is operated on under spinal anesthesia, in the waist position, through a perineal approach in 2 stages:
Colonic section: After removal of the sutures, we start with a gentle dissection of the adhesions between the anal canal and the colonic stump, which we will free and uninvaginate. The lowered colon thus mobilized, the externalized colonic end is then resected up to the pectineal line.
Colo-anal anastomosis: The colo-anal anastomosis is made manually, in separate stitches, with 3/0 slow resorption suture, between the entire colonic wall and the top of the anal canal at the pectineal line. At the end of the operation, the anastomosis is reintegrated into the anal canal and disappears from view (Figure 5).
The patient is discharged from hospital the same day or the day after the operation.
Our study included 5 patients, 4 women and 1 man with a mean age of 62.6 years. The average follow-up was 15.8 months (minimum 7 months and maximum 24 months). Post-operative follow-up: 4 of the selected patients had simple post-operative follow-ups, they left the department on day 3 post-op. One patient presented a localized ischemia of the perineal stoma on the second postoperative day without general signs of sepsis, treated by surgical revision on the third postoperative day under spinal anesthesia by the resection of approximately 3 cm of a necrotic colonic end and by the creation of a colo-anal anastomosis while keeping the pericolic reinforcement sleeve. The second stage of the operation was not used in this patient (Table 1).
| Sex | Age | Location | Recule | Clavien-dindo** | Kirwan | Level of Satisfaction | |
|---|---|---|---|---|---|---|---|
| Case 1 | Female | 63 | 4 cm from MA* | 14 months | Grade 1 | A | Very good satisfaction |
| Case 2 | Female | 56 | 2 cm from MA | 24 months | Grade 1 | B | Good satisfaction |
| Case 3 | Female | 76 | 3 cm from MA | 24 months | Grade 1 | B | Good satisfaction |
| Case 4 | Male | 68 | 2 cm from MA | 10 months | Grade 3 | C | Moderate satisfaction |
| Case 5 | Female | 49 | 3 cm from MA | 7 months | Grade 1 | A | Very good satisfaction |
Protective stoma: In all 5 cases the protective stoma could be avoided. Functional results of sphincter continence and degree of satisfaction (Table 1).
There was a progressive improvement in functional anal continence results over time.
2 patients were classified as Kirwan grade A at 7 months and 14 months follow-up with very good satisfaction
2 patients were classified as Kirwan Classification grade B over a follow-up of 24 months with good satisfaction.
1 patient was classified as Kirwan Grade C with occasional soiling and improved after irrigation with moderate satisfaction.
The third main concern after the carcinological result and the sphincter conservation of the cancer of the lower rectum is to be able to avoid the realization of a stoma, even transitory and also to improve the postoperative functional result. In the light of published results, we have speculated about the improvement of functional results after resection of tumors of the lower rectum, by associating the principle of sphincter reinforcement by a Musculo serosal flap, as described during CPC after PAA according to Shmidt, this time with sphincter in place. In addition and taking into account the complications inherent in the stoma and its psychosocial repercussions on the patients, even temporary and with a view to avoiding it during surgery for cancer of the lower-middle rectum, this new surgical procedure consisting of the creation of a primary perineal stoma associated with daily irrigation followed by a colo-anal anastomosis has multiple advantages which have been identified in our study:
• Possibility of avoiding a temporary stoma and its own morbidity.
• Effective monitoring and control of the viability of the perinealy stomached colonic stump and thus early detection and treatment of necrosis of the lowered graft.
• Sufficient time to secure adhesions between the colon and the pelvic wall thus reducing the risk of anastomotic fistula.
• Avoid abdominal scarring after restoration of stoma continuity.
• Reduce hospital stay.
• To improve the results of anal continence described as satisfactory in our study.
• Finally, the different operative steps fully respect the principles of oncology.
The preliminary results of our study are very encouraging. A comparative study between reinforced and deferred colo-anal anastomosis and classic colo-anal anastomosis, is currently underway in our surgical department.
• The retrospective nature of the study.
• Limited number of patients.
The reinforced and deferred colo-anal anastomosis is a simple and reproducible surgical technique that respects the principles of rectal cancer surgery. It is a promising technique, avoids a temporary stoma, reduces morbidity, has an aesthetic advantage by avoiding stomal scarring, reduces the hospital stay and improves anal continence. The results of this study are very encouraging. Further evaluation on a larger panel of patients is needed to validate it as a therapeutic option for lower-middle rectal cancer. A comparative study between RDCAA and conventional colo-anal anastomosis is currently underway in our surgical department.
Rectal cancer; Functional results; Protective stomia
The authors declare no conflict of interest.
[1] Ziade G, Barake Hida JI, Yoshifuji T, Matsuzaki T and Hattori T, et al. (2007). Long-term functional changes after low anterior resection for rectal cancer compared between a colonic J-pouch and a straight anastomosis. Hepatogastroenterology 54: 407-413.
Google Scholar, Crossref, Indexed at
[2] Joo JS, Latulippe JF, Alabaz O, Weiss EG and Nogueras JJ, et al. (1998). Long-term functional evaluation of straight coloanal anastomosis and colonic J-pouch: Is the functional superiority of colonic J-pouch sustained?. Dis Colon Rectum 41: 740-746.
Google Scholar, Crossref, Indexed at
[3] Lasser P, Dube P, Guillot JM and Elias D. (2001). Pseudocontinent perineal colostomy following abdominoperineal resection: Technique and findings in 49 patients. Eur J Surg Oncol 27: 49-53.
Google Scholar, Crossref, Indexed at
[4] Pocard M, Sideris L, Zenasni F, Duvillard P and Boige V, et al. (2007). Functional results and quality of life for patients with very low rectal cancer undergoing coloanal anastomosis or perineal colostomy with colonic muscular graft. Eur J Surg Oncol 33: 459-462.
Google Scholar, Crossref, Indexed at
[5] Kirwan WO, Turnbull RB, Fazio VW and Weakley FL. (1978). Pullthrough operation with delayed anastomosis for rectal cancer. Br J Surg 65: 695-698.
 Awards Nomination
Awards Nomination