2376-0249
Clinical-Medical Image - International Journal of Clinical & Medical Images (2024) Volume 11, Issue 1
Author(s): Leonardo A. Montes*, Martina Bigerna, Juan C Fasolo, Lucia Novellis, Pablo Farinelli, Pablo Barros Schelotto and Gabriel Gondolesi
Institute of Multiorgan Transplantation, Hepatobiliary Surgery and Hepatic Transplantation, Favaloro Foundation University Hospital, Belgrano Ave 1746, (1093) Buenos Aires, Argentina
*Corresponding Author:
Leonardo A. Montes
Institute of Multiorgan Transplantation
Hepatobiliary Surgery and Hepatic Transplantation
Favaloro Foundation University Hospital
Belgrano Ave 1746, (1093) Buenos Aires, Argentina
Tel: 541167878659
E-mail: leomontes04@gmail.com
Received: 01 January 2023, Manuscript No. ijcmi-24-124421; Editor assigned: 03 January 2023, Pre QC No. P-124421; Reviewed: 17 January 2023, QC No. Q-124421; Revised: 23 January 2024, Manuscript No. R-124421; Published: 31 January 2024, DOI:10.4172/2376-0249.1000935
Citation: Montes LA, Bigerna M, Fasolo JC, Novellis L and Farinelli P, et al. (2024) Minimally Invasive Management of Gastro Duodenal Aneurism. Int J Clin Med Imaging 11: 935.
Copyright: © 2024 Montes LA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Visceral Artery Aneurism (VAA) are exceptional, the most frequent is the splenic artery aneurism. With new imagenologic methods incidental diagnosis became more frequent. Although asymptomatic, abdominal pain is the predominant symptom. Cholestatic syndrome is extremely rare, there are a few described in the biography. To this day minimally invasive treatments are of choice, leaving open surgery for emergencies and patients with broken aneurysms hemodynamically instable.
Objective: We reported a case of obstructive jaundice and pruritus do to external compression by gastroduodenal artery aneurism, which was resolved entirely with minimal invasive methods.
Results: Even though our patient required multiple interventions, he was managed with endovascular and percutaneous treatments satisfactorily. 24 months post operatively the patient is stable at home without any symptoms.
Conclusion: VAA are rare, there are some reported cases associated with celiac trunk stenosis, in this case report we highlight the importance of diagnosis and minimally invasive treatment.
Visceral artery aneurysms are a rare affection; although infrequent the descripted prevalence goes from 0.01% to 2% of the population. The most frequent is the splenic aneurysm (36-36%). Gastroduodenal aneurysm represents 1-15% of VAA [1]. They have a risk of rupture of the 25% and mortality that goes up till 70% once ruptured [2].
The first case of VAA was descripted in literature in 1895 by Ferguson, et al.
Diagnosis mean age is 50 years old and male predominance its descripted with a 4.5:1 ratio [3].
Depending on the anatomy of the aneurysm they can be divided into true aneurysms or pseudoaneurysms. The first of them have compromised the three layers of the vascular wall. Meanwhile the second type have affected the two internal layers (tunica Intima and media) and the outermost layer is preserved. This generates that the turbulent blood flow is contained only by the adventitia of the artery.
The risk factors descripted for VAA are intra-abdominalinfectious diseases, arterial hypertension, diabetes, smoking, atherosclerosis, collagen diseases like Marfan or Ehlers- Danlos. ERCP, trauma or pancreatitis [4]. There’s an English revision that dates between 1970 and 1995 that ACUSA acute pancreatitis to be the first cause associated with gastroduodenal aneurysms followed by enolic habit [5].
The aim of this case report was to go through published biography and share the management of an infrequent affection with minimally invasive therapies.
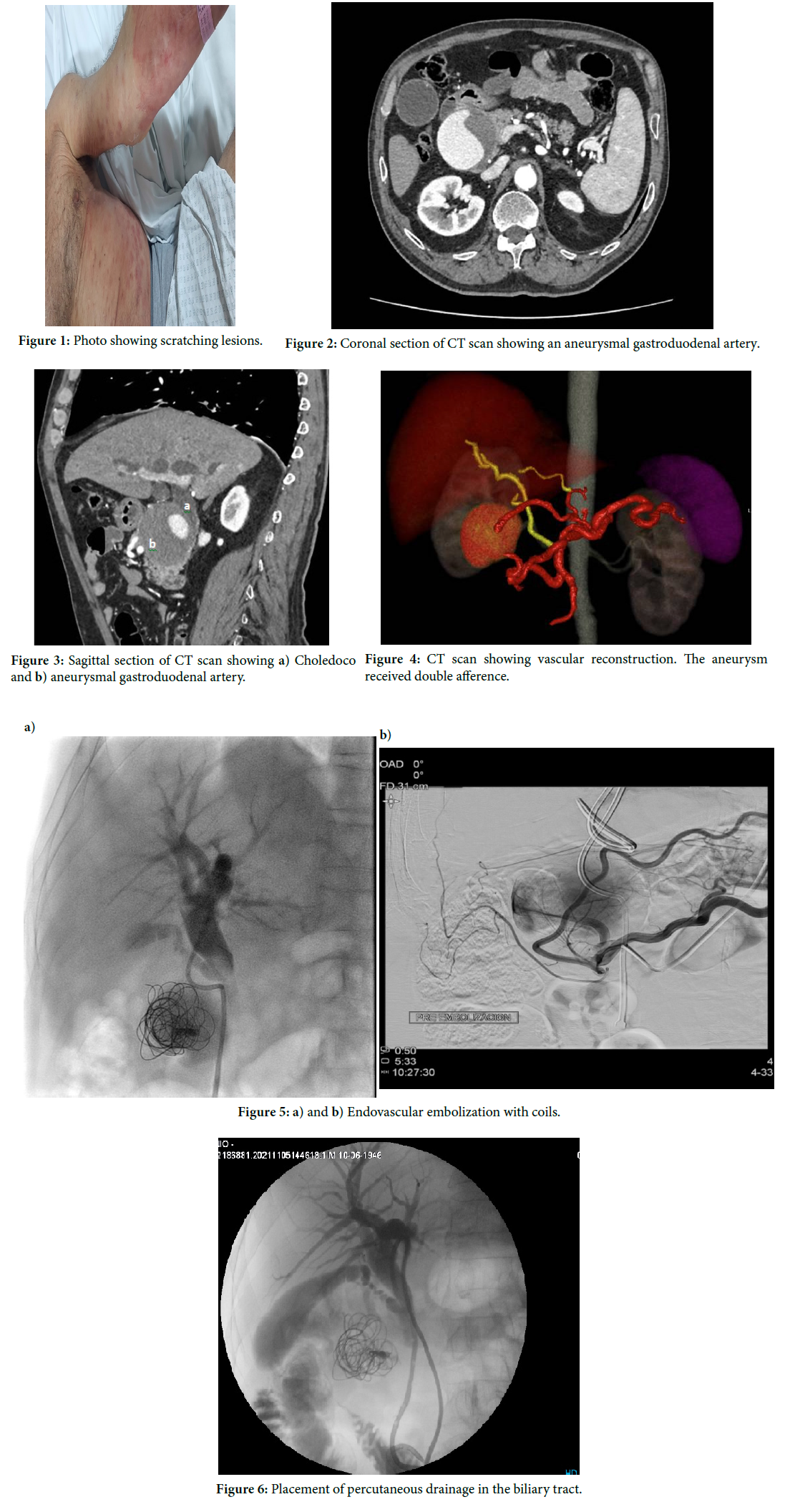
This is a 73 year old male, whose disease started with an erythematous, pruriginous cutaneous rush. He was treated by a dermatologist for a month with steroids and antihistamines, obtaining no clinical results (Figure 1).
One month after he started clinical treatment he debuted with jaundice and choluria.
In the analysis he had a cholestasic pattern (BT: 5.2 mg/dl, BD: 3.1 mg/dl, GGT: 1439 U/l. FAL: 1403 U/l). The ultrasound showed dilatated bile ducts, caused by compression of a vascularized mass located next to the pancreatic head. Doppler showed it had vascular flow and a mural thrombus.
The patient is now referred to our center with the previous studies, We completed them with an abdominal CT scan with vascular times that informs a voluminous aneurysmatic mass located in the hepatic hilium, partially thrombosed. Its measurements were 6.6 cm × 6.2 cm (Figure 2). It generated extrinsic compression of the choledocus thus causing biliary dilatation. (Figure 3). The aneurysm received double afference, from the common hepatic artery/ gastroduodenal artery and a branch that depended of the superior mesenteric artery (Figure 4).
We discussed the clinical case in a multidisciplinary meeting with vascular specialists, radiologists and surgeons and concluded that the best solution was with minimally invasive techniques with arteriography and vascular exclusion with coils under general anesthesia.
Even though risk of rupture of the aneurism, given the clinical evolution of the cholestasic syndrome we decided to start with the drainage to palliate pruritus and icterus. Secondarily to the impossibility to progress the road runner through the extrinsic stop caused by the aneurysm. We drained the biliary duct with an external biliary drainage (Cook Medical, Bloomington, IN, USA) under general anesthesia.
He presented improvement in pruritus and cholestatasic pattern hours after the procedure; he was discharged on the first postoperative day.
He attended outpatient control on the sixth day, reporting complete remission of the canalicular symptoms.
Subsequently, the AGD was embolized by the percutaneous interventionists, who excluded the gastroduodenal artery with 10 coils, Lipiodol and a Histoacrylhe was readmitted two days later due to pain in the right hypochondrium, without other accompanying symptoms. Control hepatogram: AST 28 U/l, ALT 60 U/l, FAL: 153 U/l, total bilirubin: 3.1 mg/dl, direct bilirubin: 2.4 mg/dl, GGT 503 U/l. Billiary drainage discharge with 350ml of daily debit. A control CT angiography was requested, which revealed a partially occluded aneurysm with a small endoleak and critical stenosis of the celiac trunk.
A new percutaneous procedure was performed with angioplasty of the celiac trunk and implantation of Herculink Elite 5.0 × 12 mm and 5.0 × 18 mm stents. With subsequently, embolization of the gastroduodenal artery was performed with 8 coils. The patient tolerated the procedure adequately and was discharged (Figure 5).
After the fourth postoperative month of biliary drainage, biliary dilatation and subsequent internalization of the drainage was performed (Figure 6). Control CT shows changes linked to endovascular manipulation due to embolization of aneurysmal dilatation in the cephalic portion of the pancreas dependent on the gastroduodenal artery, thrombosed, without significant changes in its dimensions, with persistence of a focus of opacification in the ventral portion dependent on the gastroduodenal artery. We performed a new cholangiography that showed a non-dilated bile duct, good passage of contrast to the duodenum, so the biliary drainage is removed and externalized.
Currently, after 24 months since the last procedure, patient remains asymptomatic, with normal labs.
Gastroduodenal aneurysms are a rare affection, 85% of them are pseudoaneurysms and the extrinsic compression of the extra hepatic duct is exceptional [6]. Psudoaneurysms are considered less stables and have a mayor risk of rupture than real aneurysms [7]. From the pathophysiological point of view aneurysms could be explained by the increase of blood flow as a compensation of celiac trunk stenosis or superior mesenteric artery [3]. Speaking of pseudoaneurysms the inflammatory local response for example after acute pancreatitis, result with the lesion of the vascular wall mediated by proteolytic enzymes [3,8,9].
Clinically aneurysms characterize by its silent evolution. When symptoms present, they are usually related with its rupture. The main symptoms are abdominal pain, hemodynamic instability, hematemesis, or melena [7]. The risk of rupture is not related with its size. When rupture happens, they usually present gastrointestinal bleeding, haemobilia or hemoperitoneum with its consequent hypovolemic shock.
There’s a revision by Habib, et al. That states that gastrointestinal bleeding secondary to an aneurysmatic rupture was the most frequent clinical presentation. Mortality will be determined by the severity of the rupture, bleeding and anatomical site of rupture. Mortality after rupture can go up to 40%. Mortality rate is reported to be higher when the aneurysm ruptures to the duodenum. They can also present themselves as retroperitoneal or intrabdominal bleeding with a risk of mortality of 19% [3]. Jaundice secondary to extrinsic compression is rare. Konstantakos, et al. Identify 17 cases of cholestasis because of compression of principal bile duct. The first cases were described in Groffin y Furhman in 1972. They described 7 cases more in the period that goes from 2001 until 2019 [7].
Prior to the advent of sophisticated diagnostic imaging methods, aneurysms were diagnosed once symptomatic or complicated. Nowadays incidental diagnosis rose.
Actual diagnostic methods include ultrasonogram with doppler, computed Angio tomography and angiography. The screening diagnostic exam is the ultrasound with doppler (S=50%) even though they are operative dependent. Pseudoaneurysms are seen like an anechoic ovoid mass, with thin walls, doppler positive with a Ying yang characteristic image. Also you can find thrombosis within its walls. These being anechoic images. True aneurysms appear to be round, hypoechogenic and with variable grades of thrombosis. During angio tomography they are correctly seen during arterial times, excluding aneurysms with strict neck. Pseudoaneurysms are seen in both arterial and venous acquisitions with a sensibility of the 65%. Magnetic resonance can be the diagnostic alternative in iodine allergic patients or in renal disfunction.
Visceral angiography is the gold standard for the diagnosis of visceral artery aneurisms, reaching to 100% in specificity, this method helps not only with diagnosis but also with its definitive treatment. This procedure has a high rate of success with low rate of morbility.
Endovascular catheter-directed treatment techniques include embolization using coils, use of closure device, or embolization using liquid embolic agents. An endovascular approach using glue (N-butyl cyanoacrylate) is commonly described as embolization technique for visceral artery pseudoaneurysms [10].
Alternative treatments include surgical approach with the aneurismatical ligation, resection of the aneurysm or vascular bypass with cadaveric or autologous vascular grafts, they can also replace vascular grafts with prothesic vascular grafts. Surgical approach is indicated once endovascular treatment fails, or when endovascular approach is not available. There isn’t a published consensus that describes surgical indications. What we know to this day is that aneurysms over 2cm that generate symptoms are to be treated. Gastroduodenal aneurysms should be treated despite its size [2,11] because of it’s high rate reported complications and risk of rupture that goes to 80% [11] and the mortality rate reaches 70% [3].
The endovascular treatment has the benefits of a minimally invasive procedure, with rapid recovery and shorter hospital stay; as a disadvantage, you need a trained team with resources available 24 hours a day.
Until the new millennium, three cases of aneurysmal embolization of the gastroduodenal artery with coils in cases of bile duct obstruction were reported. Of them, only one was successful resolved with endovascular treatment. Subsequently, 6 cases with bile duct obstruction were published, of these, 5 were successful. In 2 cases, the aneurysm reduced in size after the procedure, with the consequent resolution of the bile duct obstruction without the need for endoscopic resolution. There are two reported cases of endoscopic resolution with ERCP with papillotomy and/or stent placement [7].
Some of the reported complications of endovascular treatment are toxicity secondary to iodine contrast or complications associated to the puncture site.
For the final resolution of aneurysms it usually requires various methods or treatments.
Including the use of coils, embolic agents, coated stents and thrombin injection [12,13]. The choice of each modality will depend on the expertise of the treating team and on each case.
An infrequent case in literature has been described. Due to the symptoms and the location of the aneurysm, the mini-invasive resolution was chosen, obtaining a satisfactory clinical response. Despite having required various interventions, the patient obtained a successful outcome without resorting to open surgery with lower morbidity and mortality.
Aneurysm of the gastroduodenal artery; Cholestasis; Interventionism
There is no conflict of interest.
[1] Obara H, Kentaro M, Inoue M and Kitagawa Y. (2020). Current management strategies for visceral artery aneurysms: An overview. Surg Today 50: 38-49.
Google Scholar, Crossref, Indexed at
[2] Erben Y, Brownstein AJ, Rajaee S, Li Y and Rizzo JA, et al. (2018). Natural history and management of splanchnic artery aneurysms in a single tertiary referral center. J Vasc Surg Cases 68(4): 1079-1087.
Google Scholar, Crossref, Indexed at
[3] Habib N, Hassan S, Abdou R, Torbey E and Alkaied H, et al. (2013). Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: A concise review. Ann Surg Innov Res 7(1): 1-6.
Google Scholar, Crossref, Indexed at
[4] Gangahar DM, Carveth SW, Reese HE, Buchman RJ and Breiner MA. (1985). True aneurysm of the pancreaticoduodenal artery: A case report and review of the literature. J Vasc Surg Cases 2(5): 741-742.
Google Scholar, Crossref, Indexed at
[5] Shanley CJ, Shah NL, Messina LM. (1996). Uncommon splanchnic artery aneurysms: Pancreaticoduodenal, gastroduodenal, superior mesenteric, inferior mesenteric and colic. Ann Vasc Surg 10(5): 506–515.
Google Scholar, Crossref, Indexed at
[6] Fankhauser GT, Stone WM, Naidu SG, Oderich GS and Ricotta JJ, et al. (2011). The minimally invasive management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg Cases 53(4): 966-970.
Google Scholar, Crossref, Indexed at
[7] Shell M, Reinhart E, Smith S, DeMarris D and Naumann C. (2021). Successful minimally invasive management of a gastroduodenal artery pseudoaneurysm causing extrinsic bile duct compression. ACG Case Rep J 8(9).
Google Scholar, Crossref, Indexed at
[8] Green D and Carroll BA. (1984). Aneurysm of the gastroduodenal artery causing biliary obstruction: Realâ?Âtime ultrasound diagnosis. J Med Ultrasound 3(8): 375-377.
[9] Cui HY, Jiang CH, Dong J, Wen Y and Chen YW. (2021). Hemosuccus pancreaticus caused by gastroduodenal artery pseudoaneurysm associated with chronic pancreatitis: A case report and review of literature. World J Clin Cases 9(1), 236.
Google Scholar, Crossref, Indexed at
[10] Giragani S, Balani A, Mallu GR, Yedlapati G and Maturu VN, et al. (2019). Endovascular glue embolization for control of massive hemoptysis caused by peripheral pulmonary artery pseudoaneurysms: Report of 7 cases. Lung India: Official Organ of Indian Chest Society 36(1): 8.
Google Scholar, Crossref, Indexed at
[11] Hosn MA, Xu J, Sharafuddin M and Corson JD. (2019). Visceral artery aneurysms: Decision making and treatment options in the new era of minimally invasive and endovascular surgery. Int J Angiol 28(01): 011-016.
Google Scholar, Crossref, Indexed at
[12] Konstantakos AK, Coogan SM, Husni EA and Raaf JH. (2000). Aneurysm of the gastroduodenal artery: An unusual cause of obstructive jaundice. Am Surg 66(7): 695-698.
[13] Hemp JH, Sabri SS. (2015). Endovascular management of visceral arterial aneurysms. Tech Vasc Intervent Radiol 18(1):14–23.
Google Scholar, Crossref, Indexed at
 Awards Nomination
Awards Nomination