Abstract: Spontaneous pneumomediastinum is a rare medical condition that would be face at the emergency room. There is a wide range of differential diagnosis that explain its clinical presentation. In this case, a previous young healthy patient was presented with ear pain and odynophagia and finally diagnosed with pneumomediastinum. The objective of this manuscript is to present a rare case and review the current literature about this pathology.
Introduction: An 18 year-old female was incidentally diagnosed to have a pneumomediastinum on chest X-ray and computed tomography axial of thorax performed at the emergency room, while physicians were evaluating odynophagia and acute thoracic pain in a patient without relevant background. The clinical radiological findings are briefly discussed in this article. Case Presentation An 18-year old female patient, college student with no previous medical history arrived at the emergency department of an Academic-Based Hospital in Bogota presenting odynophagia, right earache and chest pain during the last two days. A week ago, the patient had presented the same clinical symptoms that were partially improved at home taking oral analgesics. In the current episode, symptoms presented were associated with a sudden dyspnea with spontaneous improvement accompanying with sensation of thoracic discomfort. Physical examination showed adequate general conditions, hydrated, afebrile without fever or chills, no nausea or vomiting as well as neither alterations in its level of oxygen saturation. Specific examination at the pharyngeal level, abscesses and erythema were not found, and cardiac auscultation and pulmonary fields revealed no alterations.
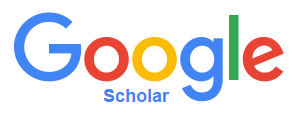
A diagnosis of typical incipient viral rhinopharyngitis was considered, for which she was ordered to perform a complete blood count, renal function labs and chest X-ray. Upon revaluation, the patient was found to have a normal blood count with normal creatinine but the chest X-ray showed subcutaneous emphysema at the base of the neck on the left side and in front of the cardiac silhouette in the lateral projection. Such findings were incidental since no pneumomediastinum was expected to be found in the context of a young patient with usual influenza-like illness without signs of systemic inflammatory response and acute respiratory failure. Based on this clinical scenario, patient was evaluated by pneumologists who considered ordering a thorax computerized axial tomography (CT Scan) to rule out lesions at the level of the airway and requested an evaluation by gastroenterology to perform an endoscopy of the upper digestive tract to rule out lesions at this level. The patient’s thorax CT Scan showed subcutaneous emphysema in soft tissues of the mediastinum and neck area without additional findings explaining a secondary origin that confirmed primary pneumomediastinum (Figure 1). Upper gastrointestinal endoscopy was performed by gastroenterologist only funding erythematous patch in a gastric antrum related with antral gastritis without suggestions of perforation that would explain the findings of the thorax CT Scan. Finally, a diagnosis of spontaneous primary pneumomediastinum was established. Due to this, a concept from cardiothoracic surgery service was requested. The patient was evaluated and favorable evolution without findings of respiratory difficulty or signs of progression of subcutaneous emphysema related to the pneumomediastinum was found. Ultimately, a conservative management was considered and the patient was discharged from the hospital with analgesic treatment and oxygen support by nasal cannula.
Clinical Scenario: Pneumomediastinum is a rare medical situation that is characterized by a wide clinical spectrum of symptom and is commonly considered an exclusion diagnosis of chest pain or less suspected. Currently, imaging techniques guide physicians to confirm this pathology [1,2]. Hamman has proposed different pathways since the first case report was published in 1939. Macklin in 1944 described the pnemomediastinum as a barotrauma, causing by alveolar rupture with consequent air dissection of the ascending bronchovascular sheat to a different areas, such as: bronchovascular pedicle, mediastinum, neck, subcutaneous tissue. There is not a clear classification, but usually depending on extension is classified (simple, severe, and complicated) [3,4]. Almost 70% of the patients have healthy lung parenchyma and a coexisting factor to increases suddenly the pulmonary pressure, most common cases are described as; severe asthma crisis, incoercible cough, exercise movements like heavy lifting practice, playing wind instruments, labour pushing or even after dental procedures [5]. Remaining 30% cases are related with any other pathologies with lung parenchyma structural modifications like chronic obstructive pulmonary disease and its wide spectrum of pulmonary complications, occupational pneumopaties, and interstitial pneumopaties. Other causes are included such as iatrogenic higher pressure applied to the different cavities: abdominal: (colonoscopy, laparoscopic surgery), thoracic: (thoracoscopy, thoracostomy), pericardic: percardiocentesis [5,6]. The common symptom related to pneumomediastinum is chest pain; remarkable for the diagnose because, bronchiolar pedicule is fully loaded of nerves that cross the area, which explain the refered pain. Actually, there is not a real number of cases or statistical reports for this pathology, due to few cases reported annually. Nonetheless at certain time, new case reports are Volume 5 • Issue 1 • IJCMI • Page 3 of 3 • being published in the medical literature. In order to achieve an adequate a precise diagnosis, the starting point as a physician is to prepare a good clinical history and a focused guided-interview that could limit the number of differential diagnoses [1,7].
Always patients with parenchymal structural induced changes like smoking, asthma, recent respiratory infection, occupational pneumopathies (silicosis, biscinosis, anthracosis, inhalated drug users and others); or genetic parenchymal structure disruption like (cystic fibrosis, bronchial dysplasia, Ehlers Danlos syndrome, Marfan syndrome, dermatomyositis and others) lead a higher probability to present spontaneous pneumomediastinum [3,5,8]. Finally, the conservative treatment is the best alternative in the majority of patients, this approach includes: supplementary oxygen if it is needed, respiratory therapy and analgesia. A small percentage of patients with remarked clinical limitation will be followed up looking for complications such as, tension pneumothorax, pneumomediastinum pneumopericardium, pneumoperitoneum, which probably needs further surgical management.
 Awards Nomination
Awards Nomination